Cosmetic Non-Surgical Rx Reconstructive Surgical Rx Squamous cell carcinoma Sebaceous cell carcinoma Malignant melanoma Trimalar (tripod) fracture Lacerations |
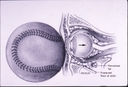
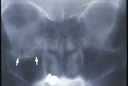
FACIAL, ORBITAL AND PERIORBITAL TRAUMATraumatic lacerations may result in injury to the face and eyelids. Precise evaluation and repair of such injuries is necessary to insure the best possible function and appearance. When a laceration involves the inner aspect of the eyelids, it is essential to determine whether the lacrimal drainage system has been severed (canalicular laceration) as this requires microscopic repair of the damaged lacrimal structures with placement of a silicone stent (Quickert tube). When a laceration involves the eyelid margin or edge of the lip (vermillion border), it is essential that these be closed in a manner that avoids irregularities such as an eyelid margin notch or lip contour abnormality. Trauma can also result in orbital or facial fractures. Such fractures may result in deformities of the face, poor movement of the eye, and may cause the eye to recede deeper into the orbit. Precise evaluation and repair are usually necessary to insure the best possible functional and cosmetic outcome. These injuries typically require Xray evaluation by specialized CT studies to reveal underlying fracture. Two of the most common fractures are (1) Orbital Floor Fracture (Blowout Fracture) and (2) Trimalar Fracture (Tripod Fracture). Blowout fracture is the most common fracture around the eye area. It is usually caused by the impact of an object (usually spherical such as a baseball or larger) against the eye or upper cheek. The force generates increased pressure within the orbit causing the orbital floor to blow out at its weakest point - the thin bony floor beneath the eye. This may cause orbital fat or one of the eye muscles to herniate toward or into the roof of the maxillary sinus which is located directly below the bony orbit. It is this potential herniation that causes the symptoms often seen in blowout fracture - double vision and/or enophthalmos (recession of the eye deeper into the eye socket). 95% of blowout fracture patients do not require surgical repair. Yet, if double vision or enophthalmos are significant and not improving at 10 to 14 days, surgery is usually indicated. This surgery can be performed using either a subciliary (skin) incision or a transconjunctival incision (through the conjunctiva without leaving a skin scar). It involves covering and closing the orbital floor bony defect with a secured implant. Trimalar fracture is usually caused by a blunt impact to the cheek resulting in fracture of the zygomatic bone. This bone has three points of attachment to adjacent bones. When one or more has been disrupted, a tripod fracture results. In many cases the cheek will immediately become malpositioned and often sunken (depressed fracture). Plain facial Xrays will often confirm the diagnosis. Most trimalar fractures require surgery once the swelling is reduced.at 7 to 10 days. This surgery is performed via a skin incision - exposing the fracture, restoring the bone to normal position, and stabilizing via titanium mini plates or wire. Blowout and tripod fracture repair are each performed under general anesthesia on an outpatient basis. Postoperative antibiotic ointment is used daily. Patients may return to normal activity within several days. |